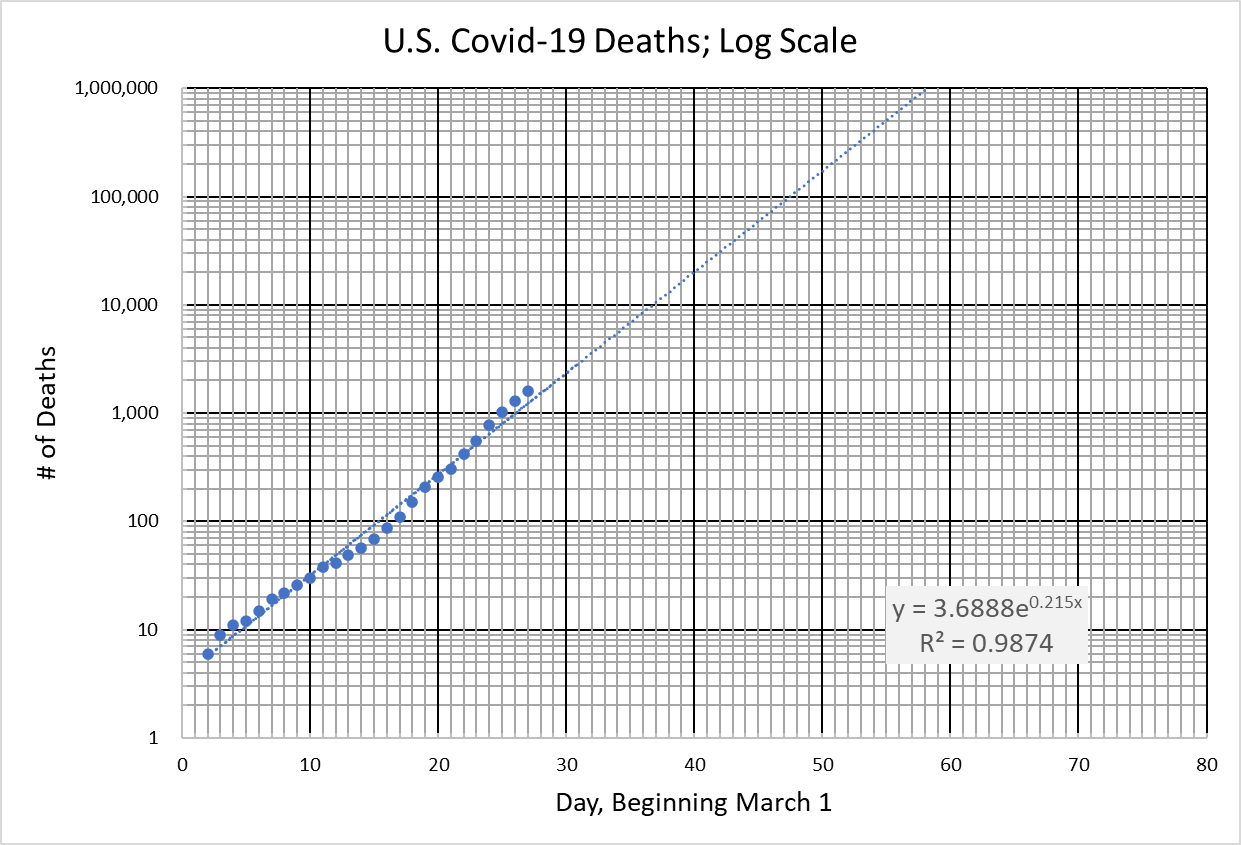
Indications are that we're headed that direction...

At the start of the coronavirus pandemic, one of the worst things about SARS-CoV-2 was that it was so new: The world lacked immunity, treatments, and vaccines. Tests were hard to come by too, making diagnosis a pain—except when it wasn’t. Sometimes, the symptoms of COVID got so odd, so off-book, that telling SARS-CoV-2 from other viruses became “kind of a slam dunk,” says Summer Chavez, an emergency physician at the University of Houston. Patients would turn up with the standard-issue signs of respiratory illness—fever, coughing, and the like—but also less expected ones, such as rashes, diarrhea, shortness of breath, and loss of taste or smell. A strange new virus was colliding with people’s bodies in such unusual ways that it couldn’t help but stand out.
Now, nearly three years into the crisis, the virus is more familiar, and its symptoms are too. Put three sick people in the same room this winter—one with COVID, another with a common cold, and the third with the flu—and “it’s way harder to tell the difference,” Chavez told me. Today’s most common COVID symptoms are mundane: sore throat, runny nose, congestion, sneezing, coughing, headache. And several of the wonkier ones that once hogged headlines have become rare. More people are weathering their infections with their taste and smell intact; many can no longer remember when they last considered the scourge of “COVID toes.” Even fever, a former COVID classic, no longer cracks the top-20 list from the ZOE Health Study, a long-standing symptom-tracking project based in the United Kingdom, according to Tim Spector, an epidemiologist at King’s College London who heads the project. Longer, weirder, more serious illness still manifests, but for most people, SARS-CoV-2’s symptoms are getting “pretty close to other viruses’, and I think that’s reassuring,” Spector told me. “We are moving toward a cold-like illness.”
That trajectory has been forecast by many experts since the pandemic’s early days. Growing immunity against the coronavirus, repeatedly reinforced by vaccines and infections, could eventually tame COVID into a sickness as trifling as the common cold or, at worst, one on par with the seasonal flu. The severity of COVID will continue to be tempered by widespread immunity, or so this thinking goes, like a curve bending toward an asymptote of mildness. A glance at the landscape of American immunity suggests that such a plateau could be near: Hundreds of millions of people in the U.S. have been vaccinated multiple times, some even quite recently with a bivalent shot; many have now logged second, third, and fourth infections with the virus. Maybe, just maybe, we’re nearing the level of cumulative exposure at which COVID gets permanently more chill. Then again? Maybe not—and maybe never.
The recent trajectory of COVID, at least, has been peppered with positive signs. On average, symptoms have migrated higher up the airway, sparing several vulnerable organs below; disease has gotten shorter and milder, and rates of long COVID seem to be falling a bit. Many of these changes roughly coincided with the arrival of Omicron in the fall of 2021, and part of the shift is likely attributable to the virus itself: On the whole, Omicron and its offshoots seem to prefer infecting cells in the nose and throat over those in the lungs. But experts told me the accumulation of immune defenses that preceded and then accompanied that variant’s spread are almost certainly doing more of the work. Vaccination and prior infection can both lay down protections that help corral the virus near the nose and mouth, preventing it from spreading to tissues elsewhere. “Disease is really going to differ based on the compartment that’s primarily infected,” says Stacey Schultz-Cherry, a virologist at St. Jude Children’s Research Hospital. As SARS-CoV-2 has found a tighter anatomical niche, our bodies have become better at cornering it.
With the virus largely getting relegated to smaller portions of the body, the pathogen is also purged from the airway faster and may be less likely to be passed to someone else. On the individual level, a sickness that might have once unfurled into pneumonia now gets subdued into barely perceptible sniffles and presents less risk to others; on the population scale, rates of infection, hospitalization, and death go down.
This is how things usually go with respiratory viruses. Repeat tussles with RSV tend to get progressively milder; post-vaccination flu is usually less severe. The few people who catch measles after getting their shots are less likely to transmit the virus, and they tend to experience such a trivial course of sickness that their disease is referred to by a different name, “modified” measles, says Diane Griffin, a virologist and an immunologist at Johns Hopkins University.
It’s good news that the median case of COVID diminished in severity and duration around the turn of 2022, but it’s a bit more sobering to consider that there hasn’t been a comparably major softening of symptoms in the months since. The full range of disease outcomes—from silent infection all the way to long-term disability, serious disease, and death—remains in play as well, for now and the foreseeable future, Schultz-Cherry told me. Vaccination history and immunocompromising conditions can influence where someone falls on that spectrum. So too can age as well as other factors such as sex, genetics, underlying medical conditions, and even the dose of incoming virus, says Patricia García, a global-health expert at the University of Washington.
New antibody-dodging viral variants could still show up to cause more severe disease even among the young and healthy, as occasionally happens with the flu. The BA.2 subvariant of Omicron, which is more immune-evasive than its predecessor BA.1, seemed to accumulate more quickly in the airway, and it sparked more numerous and somewhat gnarlier symptoms. Data on more recent Omicron subvariants are still being gathered, but Shruti Mehta, an epidemiologist at Johns Hopkins, says she’s seen some hints that certain gastrointestinal symptoms, such as vomiting, might be making a small comeback.
All of this leaves the road ahead rather muddy. If COVID will be tamed one day into a common cold, that future definitely hasn’t been realized yet, says Yonatan Grad, an epidemiologist at Harvard’s School of Public Health. SARS-CoV-2 still seems to spread more efficiently and more quickly than a cold, and it’s more likely to trigger severe disease or long-term illness. Still, previous pandemics could contain clues about what happens next. Each of the past century’s flu pandemics led to a surge in mortality that wobbled back to baseline after about two to seven years, Aubree Gordon, an epidemiologist at the University of Michigan, told me. But SARS-CoV-2 isn’t a flu virus; it won’t necessarily play by the same epidemiological rules or hew to a comparable timeline. Even with flu, there’s no magic number of shots or past infections that’s known to mollify disease—“and I think we know even less about how you build up immunity to coronaviruses,” Gordon said.
The timing of when and how those defenses manifest could matter too. Almost everyone has been infected by the flu or at least gotten a flu shot by the time they reach grade school; SARS-CoV-2 and COVID vaccines, meanwhile, arrived so recently that most of the world’s population met them in adulthood, when the immune system might be less malleable. These later-in-life encounters could make it tougher for the global population to reach its severity asymptote. If that’s the case, we’ll be in COVID limbo for another generation or two, until most living humans are those who grew up with this coronavirus in their midst.
COVID may yet stabilize at something worse than a nuisance. “I had really thought previously it would be closer to common-cold coronaviruses,” Gordon told me. But severity hasn’t declined quite as dramatically as she’d initially hoped. In Nicaragua, where Gordon has been running studies for years, vaccinated cohorts of people have endured second and third infections with SARS-CoV-2 that have been, to her disappointment, “still more severe than influenza,” she told me. Even if that eventually flips, should the coronavirus continue to transmit this aggressively year-round, it could still end up taking more lives than the flu does—as is the case now.

At the start of the coronavirus pandemic, one of the worst things about SARS-CoV-2 was that it was so new: The world lacked immunity, treatments, and vaccines. Tests were hard to come by too, making diagnosis a pain—except when it wasn’t. Sometimes, the symptoms of COVID got so odd, so off-book, that telling SARS-CoV-2 from other viruses became “kind of a slam dunk,” says Summer Chavez, an emergency physician at the University of Houston. Patients would turn up with the standard-issue signs of respiratory illness—fever, coughing, and the like—but also less expected ones, such as rashes, diarrhea, shortness of breath, and loss of taste or smell. A strange new virus was colliding with people’s bodies in such unusual ways that it couldn’t help but stand out.
Now, nearly three years into the crisis, the virus is more familiar, and its symptoms are too. Put three sick people in the same room this winter—one with COVID, another with a common cold, and the third with the flu—and “it’s way harder to tell the difference,” Chavez told me. Today’s most common COVID symptoms are mundane: sore throat, runny nose, congestion, sneezing, coughing, headache. And several of the wonkier ones that once hogged headlines have become rare. More people are weathering their infections with their taste and smell intact; many can no longer remember when they last considered the scourge of “COVID toes.” Even fever, a former COVID classic, no longer cracks the top-20 list from the ZOE Health Study, a long-standing symptom-tracking project based in the United Kingdom, according to Tim Spector, an epidemiologist at King’s College London who heads the project. Longer, weirder, more serious illness still manifests, but for most people, SARS-CoV-2’s symptoms are getting “pretty close to other viruses’, and I think that’s reassuring,” Spector told me. “We are moving toward a cold-like illness.”
That trajectory has been forecast by many experts since the pandemic’s early days. Growing immunity against the coronavirus, repeatedly reinforced by vaccines and infections, could eventually tame COVID into a sickness as trifling as the common cold or, at worst, one on par with the seasonal flu. The severity of COVID will continue to be tempered by widespread immunity, or so this thinking goes, like a curve bending toward an asymptote of mildness. A glance at the landscape of American immunity suggests that such a plateau could be near: Hundreds of millions of people in the U.S. have been vaccinated multiple times, some even quite recently with a bivalent shot; many have now logged second, third, and fourth infections with the virus. Maybe, just maybe, we’re nearing the level of cumulative exposure at which COVID gets permanently more chill. Then again? Maybe not—and maybe never.
The recent trajectory of COVID, at least, has been peppered with positive signs. On average, symptoms have migrated higher up the airway, sparing several vulnerable organs below; disease has gotten shorter and milder, and rates of long COVID seem to be falling a bit. Many of these changes roughly coincided with the arrival of Omicron in the fall of 2021, and part of the shift is likely attributable to the virus itself: On the whole, Omicron and its offshoots seem to prefer infecting cells in the nose and throat over those in the lungs. But experts told me the accumulation of immune defenses that preceded and then accompanied that variant’s spread are almost certainly doing more of the work. Vaccination and prior infection can both lay down protections that help corral the virus near the nose and mouth, preventing it from spreading to tissues elsewhere. “Disease is really going to differ based on the compartment that’s primarily infected,” says Stacey Schultz-Cherry, a virologist at St. Jude Children’s Research Hospital. As SARS-CoV-2 has found a tighter anatomical niche, our bodies have become better at cornering it.
With the virus largely getting relegated to smaller portions of the body, the pathogen is also purged from the airway faster and may be less likely to be passed to someone else. On the individual level, a sickness that might have once unfurled into pneumonia now gets subdued into barely perceptible sniffles and presents less risk to others; on the population scale, rates of infection, hospitalization, and death go down.
This is how things usually go with respiratory viruses. Repeat tussles with RSV tend to get progressively milder; post-vaccination flu is usually less severe. The few people who catch measles after getting their shots are less likely to transmit the virus, and they tend to experience such a trivial course of sickness that their disease is referred to by a different name, “modified” measles, says Diane Griffin, a virologist and an immunologist at Johns Hopkins University.
It’s good news that the median case of COVID diminished in severity and duration around the turn of 2022, but it’s a bit more sobering to consider that there hasn’t been a comparably major softening of symptoms in the months since. The full range of disease outcomes—from silent infection all the way to long-term disability, serious disease, and death—remains in play as well, for now and the foreseeable future, Schultz-Cherry told me. Vaccination history and immunocompromising conditions can influence where someone falls on that spectrum. So too can age as well as other factors such as sex, genetics, underlying medical conditions, and even the dose of incoming virus, says Patricia García, a global-health expert at the University of Washington.
New antibody-dodging viral variants could still show up to cause more severe disease even among the young and healthy, as occasionally happens with the flu. The BA.2 subvariant of Omicron, which is more immune-evasive than its predecessor BA.1, seemed to accumulate more quickly in the airway, and it sparked more numerous and somewhat gnarlier symptoms. Data on more recent Omicron subvariants are still being gathered, but Shruti Mehta, an epidemiologist at Johns Hopkins, says she’s seen some hints that certain gastrointestinal symptoms, such as vomiting, might be making a small comeback.
All of this leaves the road ahead rather muddy. If COVID will be tamed one day into a common cold, that future definitely hasn’t been realized yet, says Yonatan Grad, an epidemiologist at Harvard’s School of Public Health. SARS-CoV-2 still seems to spread more efficiently and more quickly than a cold, and it’s more likely to trigger severe disease or long-term illness. Still, previous pandemics could contain clues about what happens next. Each of the past century’s flu pandemics led to a surge in mortality that wobbled back to baseline after about two to seven years, Aubree Gordon, an epidemiologist at the University of Michigan, told me. But SARS-CoV-2 isn’t a flu virus; it won’t necessarily play by the same epidemiological rules or hew to a comparable timeline. Even with flu, there’s no magic number of shots or past infections that’s known to mollify disease—“and I think we know even less about how you build up immunity to coronaviruses,” Gordon said.
The timing of when and how those defenses manifest could matter too. Almost everyone has been infected by the flu or at least gotten a flu shot by the time they reach grade school; SARS-CoV-2 and COVID vaccines, meanwhile, arrived so recently that most of the world’s population met them in adulthood, when the immune system might be less malleable. These later-in-life encounters could make it tougher for the global population to reach its severity asymptote. If that’s the case, we’ll be in COVID limbo for another generation or two, until most living humans are those who grew up with this coronavirus in their midst.
COVID may yet stabilize at something worse than a nuisance. “I had really thought previously it would be closer to common-cold coronaviruses,” Gordon told me. But severity hasn’t declined quite as dramatically as she’d initially hoped. In Nicaragua, where Gordon has been running studies for years, vaccinated cohorts of people have endured second and third infections with SARS-CoV-2 that have been, to her disappointment, “still more severe than influenza,” she told me. Even if that eventually flips, should the coronavirus continue to transmit this aggressively year-round, it could still end up taking more lives than the flu does—as is the case now.